Are your prepared for the cold and flu season? You might be feeling fine right now but even the healthiest of us can succumb to a stray virus at this time of year, resulting in days off work and…even worse…keeping you indoors and missing out on the things you love to do. Fortunately there are some surprisingly helpful little microbes you may not know about that are your winter allies – capable of helping your immune system search out viral invaders and reducing the chance of an infection taking hold. These little microbes are probiotics.
Knowing the Strain is the Key to Choosing the Right Probiotic
It’s become common knowledge that probiotics can help with gut function and digestive health – that’s perhaps what they are best known for. What you may not know though is your gut contains approximately 70% of your body’s immune system, and knowing that, you may not be so surprised to hear that certain probiotics can influence the activity of your immune cells. So how do you know which ones these are?
First you need to understand that there are many different beneficial probiotics available and each one has a different role to play in human health.
As such, the way to make sure you are using the right probiotic for your needs is to check the specific genus, species and strain (see Figure 1) has been used in human clinical trials for the condition you want to use it for – in this case reducing the likelihood of you contracting a cold or flu – because not every probiotic would be indicated for this condition.
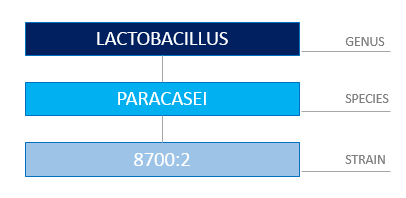
Figure 1: Correctly Identifying a Probiotic Requires You to Know the Genus, Species and Strain.
You may be wondering how a probiotic can enhance immune system function. To begin with, the microbial life living within your gastrointestinal tract (known as your gut microbiota) play an important role in maintaining the lining of your gut, which itself forms an intestinal defense barrier – so that’s one of the ways many probiotics can help – by supporting the health of the microbiota already residing within you.
However, certain probiotic strains have the ability to actually communicate directly with your immune cells, thus influencing and improving the immune response.
Two of these probiotic strains are Lactobacillus rhamnosus (LGG®) and Lactobacillus paracasei8700:2 both of which increase the activity of immune cells called natural killer (NK) cells – who, as their name suggest, actually target and kill virally infected cells – exactly what you want to tackle a cold or flu.
In addition, Lactobacillus paracasei 8700:2 and Lactobacillus plantarum HEAL 9 are two specific strains that stimulate other white blood cells (called ‘macrophages’) to secrete an important chemical signal that alerts your immune system to mount an antiviral immune response. Lastly, Lactobacillus plantarum HEAL 9, Lactobacillus paracasei 8700:2 and LGG® all have the capacity to trigger a natural chemical messenger inside your body called interleukin-10, which is a key anti-inflammatory and immune-regulating signal. Now that may all seem quite technical but what it helps demonstrate is that, used together, these three probiotic strains play a valuable role in supporting healthy immune system function.
Where’s the Evidence?
This isn’t all just theory; the ability of Lactobacillus plantarum HEAL 9 and Lactobacillus paracasei8700:2 to improve immune function has been demonstrated in a randomised, controlled trial. Two hundred and seventy-two healthy adults were given 500 million CFU* each of Lactobacillus plantarumHEAL 9 and Lactobacillus paracasei 8700:2, or placebo, for 12 weeks. Those in the treatment group experienced fewer incidences of the common cold, with significantly reduced duration and symptom severity when infection did occur. A combination of these two specific strains has also been shown to reduce symptom severity and duration of the common cold in subjects who are prone to recurrent infections.
What this all tells you is these probiotic strains have actually been tested in real situations and shown to be helpful in not only preventing colds and flus but, when someone got sick, they reduced the numbers of sick days taken – essentially the people taking these probiotic strains recovered faster.
Prevention is Better Than Cure
Don’t wait until you get sick this year, or assume there is nothing you can do about it. If you have a history of frequent colds and flus (or maybe you were one of the people who succumbed to that debilitating flu that did the rounds in Australia in 2017), don’t just pop to the pharmacy and grab any probiotic; be strategic and speak to your Healthcare Practitioner first, and ask them how best to improve your immune surveillance with probiotic strains proven to enhance immunity.
You can also help support yourself by managing your stress levels (stress depletes your immune system), eating plenty of colourful vegetables and fruits, nuts and seeds (to improve your overall nutritional status), and look after your gut health – remember, the gut is where much of your immune system is located. Take practical steps now to reduce the likelihood of you getting sick this winter, and enjoy the colder months healthy and well.
* CFU means ‘colony forming units’ and is what tells you these were live bacteria. Either CFU or ‘live bacteria’ are important things to look for on a probiotic label so you know the product contains viable organisms. Also – the specific strain must be listed on the label – if it is missing then don’t use the probiotic…you don’t know what it is!